Body Fluid Balance

Water Balance - Homeostasis
-
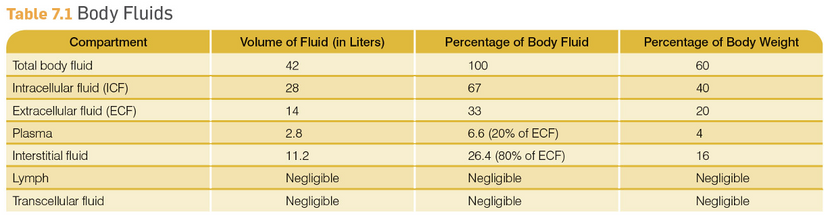
Water compartments—2 major reservoirs
-
Intracellular (28 L in reference man) -ICF
-
All water internal to cell membranes
-
-
Extracellular (14 L in reference man)-ECF
-
Plasma (cell-free intravascular compartment)
-
Interstitial Fluid
-
Bathes the extravascular cells
-
Provides a medium for passage of nutrients from blood to cells
-
Other spaces in body (pericardial, pleural, peritoneal, etc)
-
-
-
-
Homeostasis - the tendency of animals to regulate and maintain relative internal stability
-
Temperature
-
Osmotic concentration
-
pH
-
oxygen
-
CO2
-
Glucose
-

Osmosis
-
Have 2 compartments separated by a semipermeable membrane
-
Each compartment has water and solutes
-
Solutes are solid particles (proteins, electrolytes, glucose, etc)
-
-
One compartment has more solutes than the other
-
The membrane is semi-permeable
-
Lets water pass through but not the solutes that aren’t soluble in water
-
-
Water will move from the compartment with low solute concentration to the compartment with higher solute concentration
-
Goal: To get both compartments with same solute concentration (equilibrium)
-

Osmosis Terminology
-
Osmotic pressure: the pressure that must be applied through a semipermeable membrane from a solution of lower solute concentration to a solution of higher solute concentration.
-
Proportional to the number of solute particles per unit volume
-
Expressed as osmolarity
-
-
Osmolarity = # particles in solution
-
Regardless of the size of the particles
-
e.g. storage of glycogen rather than free glc
-
-
Hydrostatic pressure
-
-
Due to the pumping of the heart
-
Higher on arteriole side
-
-
Osmotic pressure (Colloidal osmotic pressure)
-
Because there are proteins in the plasma that can’t cross the barrier (capillary endothelial surface)
-
Plasma in capillaries has higher osmotic pressure than fluid in interstitial space
-
So plasma will always have these big particles which gives plasma higher osmotic pressure
-
These proteins and other large molecules are referred to as colloids
-
-
study question:
-
what is the difference between osmolarity and osmolality?
The Donnan-Equilibrium


study questions:
-
What is the Donnan equilibrium, and how does it affect the distribution of ions across a semi-permeable membrane?
-
How does the presence of impermeable ions on one side of a semi-permeable membrane influence the movement of permeable ions according to the Donnan equilibrium?
Localized Water Balance
-
Water distribution across capillary surface is controlled by a balance of forces
-
Filtration forces—move water form plasma to interstitial
-
Reabsorption forces—move water from interstitial to plasma
-
-
Based on differences in pressure between the two compartments
-
Will get into more detail during kidneys (scroll down)

Starling Forces
-
Forces for bulk flow: hydrostatic and osmotic pressures
-
Hydrostatic pressure gradient = force due to fluid
-
Osmotic pressure = osmotic force exerted on water by non-permeating solutes
-
Only non-permeating solute = proteins
-
Oncotic pressure = osmotic force of proteins
-

Water Balance

-
Filtration forces—pushes water out
-
Hydrostatic pressure (caused by pumping heart (blood pressure) = major force
-
Interstitial fluid colloidal osmotic pressure = weaker force (because not much protein in interstitial fluid)
-
study question:
-
Explain the role of hydrostatic pressure and interstitial fluid colloidal osmotic pressure in the process of filtration. How do these forces contribute to the movement of water in and out of the capillaries?
-
Reabsorption Forces (countering filtration forces)—sucks water back in
-
Plasma osmotic pressure (due to proteins)
-
At arteriole end of capillary, hydrostatic pressure higher
-
Net filtration of water into interstitial
-
-
At venule end of capillary, hydrostatic pressure significantly reduced, but plasma protein (colloidal osmotic pressure of capillary) is increased
-
Net reabsorption of water into plasma
-
-
-
Movement of water from plasma (capillaries) to interstitial fluid compartment
-
Based on differences in osmotic pressure between the two compartments
-
Plasma in capillaries has higher osmotic pressure than fluid in interstitial space
-
Because there are proteins in the plasma that can’t cross the barrier
-
So plasma will always have these big particles which gives plasma higher osmotic pressure
-
-

study question:
-
How does body maintain appropriate water content despite wide swings in intake and variation in losses via sweat and lungs? Think about which organs absorb and/or filter water
Normal

Shock: Decreased BP at Capillaries

Starvation: Decreased Osmotic Pressure due to loss of proteins

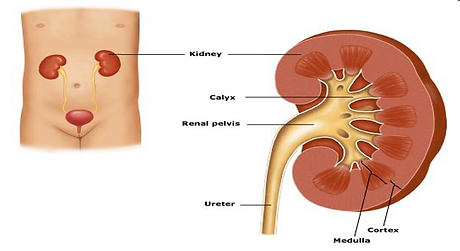
Kidney
Functions
-
Regulation of extracellular volume
-
Regulation of osmolarity
-
Regulation of ion concentrations
-
Regulation of pH
-
Excretion of wastes and toxins
-
Production of hormones
-
Erythropoietin, which stimulates RBC synthesis
-
Renin, which controls salt and water balance and blood pressure
-
Regulation of plasma calcium and glucose levels
-
-
functional unit - nephron
-
Blood from arterial supply enters glomerulus
-
Glomerulus (Bowman’s capsule) = filter
-
-
Filter = capillary network
-
Holds back RBC, WBC, proteins
-
Filters small molecules (water soluble)
-
Nutrients: glucose, amino acids, vitamins, minerals
-
Wastes: urea
-
-
-
Filtered fluid = filtrate—not all waste
-
Filtrate is on its way to becoming urine
-
-
Kidney tubules are surrounded by blood capillaries
-
Tubules have 3 segments
-
Proximal convoluted (twisted)—large area of contact with capillaries
-
Henle’s loop (deep)
-
Distal convoluted
-
-
-
The filtrate is modified as passes through tubule
-
Ends with collecting duct then goes to bladder

study question:
-
Describe the journey of blood through the nephron and explain how the filtration process works, highlighting the role of different parts of the nephron in forming urine.
-
Tubular reabsorption
-
Many small particles that leave after filtration are useful nutrients
-
Glucose, amino acids, water-soluble vitamins
-
-
These must be reabsorbed into the blood
-
Say “reabsorbed” because they started in the blood
-
-
-
Tubular secretions
-
These will leave the body in urine
-
Nitrogenous waste: urea, creatinine
-
-

Basic Renal Processes


-
Glomerular filtration—from glomerulus
to Bowman’s capsule -
Reabsorption—from tubules to peritubular capillaries
-
Secretion—from peritubular capillaries
to tubules -
Excretion—from tubules out of body
Starling Forces and Glomerular Filtration
-
Glomerular capillary hydrostatic pressure
-
Bowman’s capsule oncotic pressure
-
Bowman’s capsule hydrostatic pressure
-
Glomerular oncotic pressure
Kidney and Water Balance
-
Sensitive monitoring system in brain (hypothalamus)
-
Senses osmolarity
-
-
If increase particles vs water
-
= concentrated (dehydration)
-
-
Brain senses the need to conserve or retain water
-
Releases AntiDiuretic Hormone (ADH, also called vasopressin)

Other Renal Homeostatic Functions - Electrolytes
-
Electrolytes
-
Na+ is filtered by kidney and mainly reabsorbed
-
Cl- “goes along”
-
Na+ is key factor in ECF osmolarity (osmotic balance)
-
Process is very complex
-
Key hormone = Aldosterone
-
secreted by adrenal gland (cortex)
-
Increases renal reabsorption of Na+ when body (adrenal) senses Na+ decrease
-
Na+/ K+ ATPase
-
-
K+ is key ICF ion
-
Reabsorbed in proximal tubule
-
Then adjusted in distal tubule
-
Exchange with Na+
-
Also related to H+ excretion
-
H+/ K+ ATPase
-
-



